Biochemical mechanisms for harm are uncertain
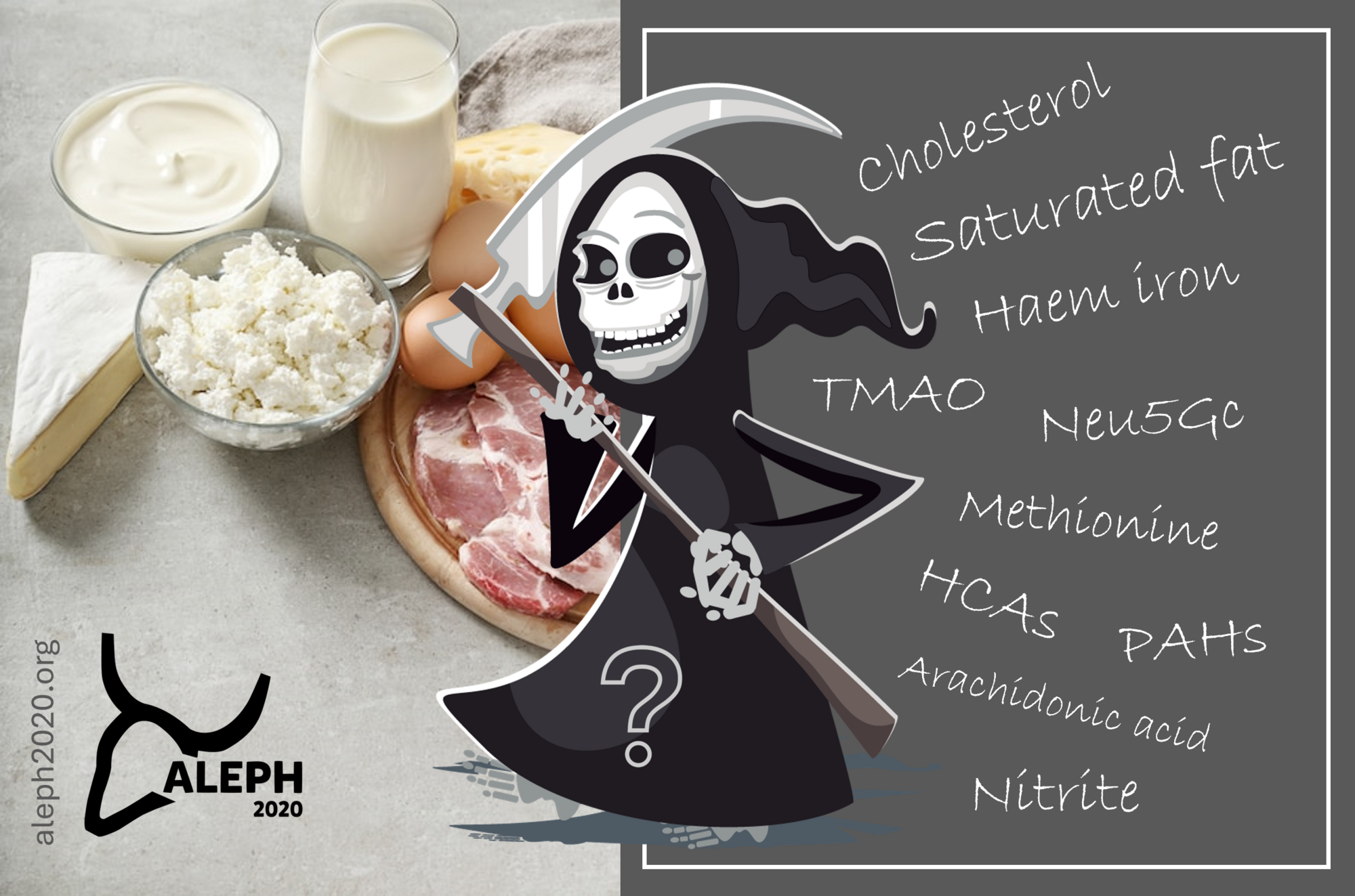
This subsection contextualizes the various potential mechanisms for harm that have been proposed to explain associations between the intake of animal source foods and disease [Hammerling et al. 2016; Jeyakumar et al. 2017; Nordhagen et al. 2020; De Smet & Van Hecke 2024]. As shown below, these mechanisms are largely unproblematic, except for some predisposed populations or when the application of excessive food processing exerts a clear harmful effect. In all cases, a distinction needs to be made between potential hazards and actual risks.
Saturated fat and dietary cholesterol
Saturated fat and dietary cholesterol in animal source foods have often been vilified due to concerns about their potential to increase serum cholesterol levels and the associated risk of cardiovascular disease. However, the relationship between these factors and disease risk is complex and not necessarily causal. Moreover, most of the recent meta-analyses have either negated or downplayed the impact of saturated fat on cardiovascular and mortality risk. In any case, the evidence is not as strong - and certainly more nuanced - as once thought. Replacing saturated fat with other nutrients is not necessarily beneficial and may even lead to worse outcomes, whereas advice to choose low-fat over whole-fat dairy is not supported by evidence (if anything, the latter seems more beneficial). Dietary recommendations are outdated and should be revised.
Haem iron
Haem iron from red meat has been associated with risks. Excessive iron consumption can elevate plasma ferritin levels, which may then be linked to adverse outcomes like oxidative stress and ferroptosis, leading to disturbances in insulin metabolism and atherosclerosis. However, this is likely not a concern for healthy individuals within a wholesome dietary context. Iron is usually kept within safe limits by bodily homeostasis, except for individuals who have genetic predispositions or metabolic disturbances. In this case, a precautionary principle of limiting iron levels may be advisable, either by eating less red meat or by blood letting. Moreover, the association between ferritin and cardiometabolic disease is inconsistent. Another point of concern is that in vitro and rodent models seem to suggest that high iron exposure could promote colorectal cancer by inducing lipid peroxidation, inflammation, cellular damage, and genotoxicity. Such studies, however, usually rely on unrealistically high levels of exposure and a dietary context that is not typical in human healthy diets, insufficiently taking into account the presence of chemoprotective compounds. Colorectal cancer risk related to iron intake might also differ by dietary source, sex, and specific individual vulnerabilities. According to the WCRF, 'the evidence suggesting that the consumption of foods containing haem iron increases the risk of colorectal cancer is limited'.
Sialic acid N-glycolylneuraminic acid
The idea that Neu5Gc, a signalling molecule in mammalian cells and present in meat and milk, would trigger human antibodies and thereby cause inflammation is speculative. Given that red meat has been a part of human evolutionary diets, such speculation seems highly unlikely.
Trimethylamine N-oxide
The conversion of L-carnitine (from meat) or choline (from eggs) into TMAO has been proposed as a mechanism leading to atherosclerosis, but this is likely a red herring. The biological role of TMAO needs to be cautiously considered within a context of complex interactions between diet, gut microbes, and the host. The case becomes more complex when considering the protective effects of fish, which contributes significantly more TMAO than other sources such as meat. Moreover, some studies found no connection between meat and TMAO, especially in a healthy dietary context, while TMAO levels rose in parallel with less healthy plant-based diets. In pigs, a prudent diet with red and processed meat resulted in lower TMAO excretion compared to the same meat-based approach combined with a Western-type background diet. The link between diet, TMAO, and disease is intricate and not as straightforward as it may appear. Factors like cardiometabolic and kidney diseases can elevate TMAO levels, suggesting that observational evidence may be influenced by confounding or reverse causality.
Gut microbiota
While the impact of animal source foods on the gut microbiota has been sometimes been portrayed as negative, compared to plant-based diets, this notion has been challenged by an intervention study. Adopting healthy diets lead to a positive shift in gut microbial composition and improved blood lipid profiles, regardless of the inclusion of unprocessed or processed lean red meats. This suggests that the relationship between animal source foods, gut microbiota, and health outcomes is less harmful (if at all) and certainly more complex than often assumed.
Protein excess
The notion that high-protein diets harm kidney and bone health in humans and may promote cancer and type-2 diabetes is not supported by robust evidence in the case of healthy humans. If anything, a generous intake of high-quality protein seems to promote rather than deteriorate health, especially in populations with higher needs, such as older adults. Although animal source foods are rich in certain amino acids like leucine and methionine, which - as such - can theoretically accelerate oxidative stress and aging in excess, there is no clear evidence that this would have harmful effects on cancer risk in healthy humans eating wholesome diets. Moreover, potential negative effects of high-methionine diets can be balanced by higher glycine intake, available through nose-to-tail eating. With respect to type-2 diabetes, there is insufficient evidence for a risk increase with higher intake of animal protein or a risk decrease with plant protein intake, which suggests a lack of effect of protein per se.
Omega-6 fatty acids and arachidonic acid
Omega-6 fatty acids present in eggs and meats have been (speculatively) linked to inflammation and carcinogenicity. However, the content and types of omega-6 fatty acids, as well as the omega-6/omega-3 ratio, depend on animal feeding methods. Moreover, how all this translates into actual and generalizable health outcomes is uncertain and a topic of debate. Arachidonic acid (AA), an omega-6 fatty acid present in eggs and meats, is sometimes speculatively linked to inflammation and carcinogenicity, although it can also be anti-inflammatory. Consumption of red meat has been associated with circulating AA levels in Chinese adults, which is attributed to pre-formed AA intake rather than its precursor linoleic acid.
Food processing
Meat processing may create potential carcinogens due to intense smoking or heating (HCA and PAH) or curing (N-nitroso compounds). Yet, evidence on their impact through human diets is mixed. The case against 'processed' meats may be less alarming than often stated. It stigmatizes a very heterogenous group of foods, many of which offer a lot of valuable nutrition per serving. The 'ultra-processed' variants, however, do require caution. Sodium, often high in processed meats, conflicts with dietary guidelines, but the link between salty foods and health risk is not conclusive for normotensive populations.
A 'hazard' is not necessarily a 'risk'
There is a lack of consistent evidence establishing a direct causal link between the consumption of red and processed meats and chronic diseases, such as colorectal cancer. Despite the International Agency for Research on Cancer (IARC) classifying red and processed meats as (probable) carcinogenic hazards, this classification does not necessarily equate to equal levels of risk as other known carcinogens. Indeed, risk assessment suggests that hazards may not translate into significant risks against reasonable dietary backgrounds. Whether or not a dietary hazard, such as red meat, also poses an actual health risk cannot be readily answered without a dedicated risk assessment. A risk is the complex outcome of a specific hazard combined with exposure (intake dose, preparation method, dietary context, etc.) and vulnerability (individual predispositions). Harms should also be weighed against benefits (e.g., nutritional value). Criticisms have emerged against IARC-type hazard classifications, highlighting issues with methodology, expert conflicts, and outdated approaches that can lead to unnecessary health concerns and adverse consequences.
